Your Ovaries’ Retirement Plan, Broken Down Step by Chaotic Step.
Darling, let’s get one thing straight: menopause doesn’t just rock up one Tuesday morning like an unannounced houseguest. Instead, it unfolds in phases, stages, and shifts so subtle you’ll wonder if you’re imagining things. (Spoiler: you’re not.)
That’s why we need the STRAW+10 stages explained, because one minute you’re cruising along, and the next, you’re knee-deep in confusion, contradictions, and moments that feel downright baffling.
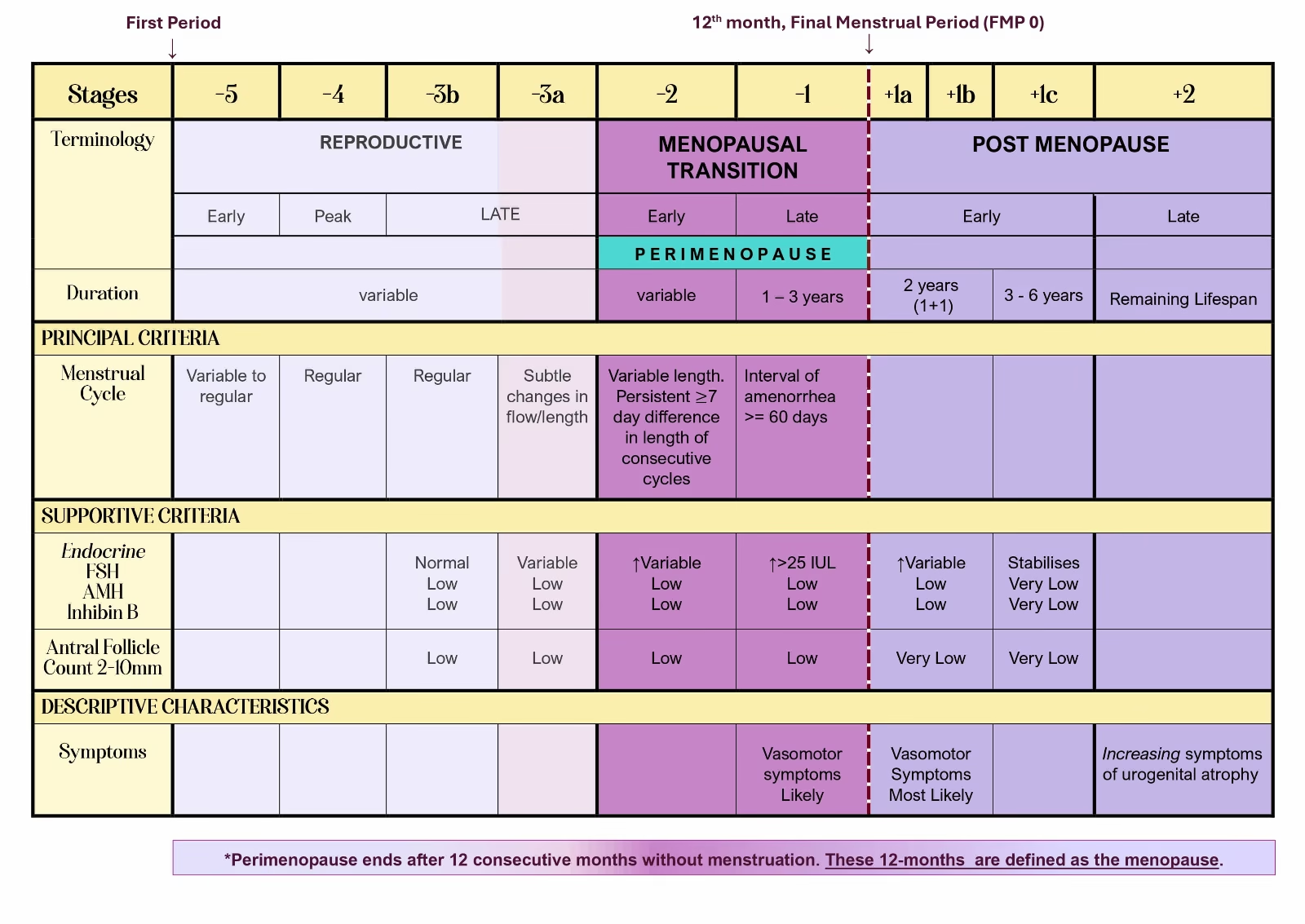
STRAW+10 Stages and Phrases
(click to enlarge image)
What This Page Covers
This page is your sanctuary from that confusion. Your calm in the hormonal storm. Your “finally, someone’s explaining this properly” moment.
We’re using the STRAW+10 framework, and before your eyes glaze over at the scientific terminology, stay with me. Because this is the internationally recognised system that actually makes sense of reproductive ageing.
Think of it as the architectural blueprint beneath the messy, beautiful, occasionally infuriating experience of menopause. Not what it feels like (we’ll get to that elsewhere, honey), but how it’s structured.
How We’ll Break It Down
I’m going to walk you through the phases and stages of menopause clearly, thoroughly, and without the medical overcomplication that makes you want to throw your laptop out the window.
You’ll see how menopause divides a woman’s life into three main phases: reproductive (when everything’s humming along nicely), menopausal transition (perimenopause, when things get interesting), and postmenopause (your grand finale and new beginning, all rolled into one).
Here’s what this isn’t: a diagnosis. A symptom checklist. A “tick these boxes and we’ll tell you where you are” quiz.
But we do have a quiz if you’d like to know what stage of perimenopause you are in. Just 5 questions, takes 5 minutes. Click here to start the quiz.
This is a clear, steady, no-nonsense explanation of the stages. Therefore, you can place yourself on the map wherever you happen to be standing right now, coffee in hand, wondering what fresh hell your body’s cooking up next.
When Does Menopause Start? Understanding Timing with STRAW+10
Now, honey, let’s talk timing. Because if there’s one thing menopause loves, it’s keeping us on our toes! While the average age for reaching menopause is 51, Mother Nature clearly never got the memo about playing by the rules.
Menopause can naturally waltz in anytime between the ages of 40 to 58. Some women hit menopause at 45 and think, “Well, this is early!” Meanwhile, others cruise past 55 still wondering when the party’s going to start!
To make sense of this gloriously unpredictable journey, the STRAW+10 system offers the 3 phase structured approach to reproductive aging mentioned above.
Think of it as Act One, Act Two, and Act Three of your own personal Broadway show. Minus the jazz hands, plus the occasional hot flash!
By clearly defining these phases and their specific stages, STRAW+10 helps women and healthcare providers identify exactly where you are in this magnificent production.
This enables more personalized and effective management of menopause symptoms and health plans. No more wondering if you’re coming or going, sweetheart. Just beautiful clarity!
Here’s the plot twist though, ma chérie: while most women move steadily from one stage to the next like a well-behaved conga line, some experience a “see-saw” effect. You might bounce back and forth between stages like you can’t decide which party to attend. Or even skip a stage entirely as if menopause is playing hopscotch with your hormones. Your body’s writing its own adventure novel, darling.

The 3 Phases & 7 Stages of STRAW+10
Reproductive Phase This phase includes the early, peak, and late reproductive stages. Basically, when your ovaries are still showing up for work with their lunchboxes packed. In the late reproductive stage, changes in the menstrual cycle and hormone levels start to occur. Fertility begins its graceful decline. Think of it as your ovaries starting to think about retirement planning!
Menopausal Transition Phase During this phase, menstrual cycles become as irregular as a teenager’s sleep schedule. Symptoms like hot flashes and mood swings often make their grand entrance. Hormonal changes such as low estrogen and fluctuating FSH levels are common. Welcome to the rollercoaster, darling. Where the only predictable thing is unpredictability!
Postmenopause Phase This phase begins after your final menstrual period (cue the confetti!). Hormone levels, including estradiol and FSH, finally stabilize like guests settling into their seats before the show. However, the risk of issues like osteoporosis and cardiovascular disease can increase due to low estrogen levels. So this is when we need to be extra vigilant about our health, ma chérie.
Now, these three fabulous phases include a total of seven stages. All centered around the final menstrual period (FMP, Stage 0). Think of the FMP as the main event, with everything else revolving around it like planets around the sun!
Reproductive Phase:
Duration: Variable (because your body doesn’t believe in one-size-fits-all!)
Stage -5: Early reproductive – (Typically teens to late 20’s) This stage kicks off with menarche. That’s your first period, darling, when you officially joined the menstruation club (membership: non-negotiable). During those first few years, menstrual cycles are often as irregular and unpredictable as British weather.
Cycle length can vary wildly. Anovulatory cycles (that’s cycles without ovulation, sweetie) are perfectly common. As time marches on, cycles generally become more regular. Though some variability may persist. Your body’s still figuring out the rhythm!
Stage -4: Peak reproductive – (Late teens to late 20’s) Ah, the golden years! During this phase, menstrual cycles typically stabilize and become more regular than your morning coffee routine. Most cycles are ovulatory. You’re experiencing your peak fertility – you’re basically a baby-making machine, whether you want to be or not!
Cycle length usually settles into a consistent pattern, often ranging from 21 to 35 days. This is your reproductive sweet spot, honey!
Stages -3b / 3a: Late reproductive – (Early 30’s to early 40’s) Here’s where things start getting interesting. During this stage, fertility begins its gentle decline while cycles remain regular. But subtle changes are brewing beneath the surface. Like a plot twist you didn’t see coming. This stage is divided into two sub-stages, because apparently one wasn’t complicated enough!
- Stage 3b: Menstrual cycles remain regular and FSH levels are still playing nice and normal. However, other indicators of ovarian health start to decline. Such as AMH (Anti-Müllerian Hormone) and AFC (antral follicle counts). Like guests leaving a party early. This decrease, along with low levels of inhibin-B observed in some studies, signals the early whispers of diminishing egg supply. Your ovaries are starting to think about winding down operations!
- Stage 3a: Subtle changes in your menstrual cycle begin to appear. Particularly shorter cycles (because apparently your body’s in a hurry now!). FSH levels increase above normal. While AMH, AFC, and inhibin-B remain low. Your hormones are having a committee meeting to discuss the transition plan!
Menopausal Transition Phase (PERIMENOPAUSE):
The menopausal transition is the critical phase that marks your shift from the reproductive years to menopause. Think of it as the intermission before the grand finale, darling. It’s divided into two key stages. And buckle up, because this is where things get properly interesting!
Stage -2: Early Menopause transition – (Early to mid 40’s) Duration: Variable (your body’s on its own schedule, honey!) Symptoms: See List
Here’s where your menstrual cycles start acting like a moody teenager. Irregular with the gap between cycles varying by 7 days or less. This pattern needs to repeat within 10 cycles to officially signal that menopause is knocking on your door.
Meanwhile, FSH levels are elevated but fluctuating like your mood after a glass of wine. While AMH and AFC levels are low. These hormonal changes reflect the declining ovarian function typical of this transition period. Your ovaries are starting their farewell tour, sweetie!
Stage -1: Late Menopause transition – (Mid 40’s to early 50’s) Duration: Typically lasts 1-3 years (though it might feel longer, darling!) Symptoms: See List
This stage is characterized by the absence of menstruation (amenorrhea) for 60 days or more. Basically, Aunt Flo has started ghosting you! During this period, menstrual cycles become as irregular as a cat’s affection. With significant hormone fluctuations and frequent anovulation (that’s when there’s no ovulation or egg release, honey).
FSH levels can vary more wildly than your cravings during this stage. They may be high (screaming “menopause is here!”). Or low if estradiol is high, which can suppress FSH levels like a bossy older sister. AMH drops to very low or undetectable levels. Basically, your ovarian reserve is running on fumes.
This stage signifies that your body is nearing the end of its reproductive years. The curtain is coming down, ma chérie!
Menopause
Menopause (Stage 0): This is it, darling – the main event! Menopause is defined as the final menstrual period (FMP) and is confirmed after 12 consecutive months without menstruation. It typically occurs in women in their late 40s to early 50s. Though as we know, some ovaries didn’t get the memo about standard timing!
This pivotal moment is marked by significant hormonal changes. Including a sharp decline in estradiol levels and a rise in follicle-stimulating hormone (FSH) levels. Your reproductive system has officially retired, honey. Time to throw it a fabulous retirement party!
Postmenopause Phase:
Duration: 5-8 years (and then some!) Symptoms: See List
Menopause, typically occurring at an average age of 51 in Western countries, marks the final menstrual period (FMP). It’s confirmed after 12 months without menstruation. One full year of freedom from tampons, darling!
During this time, FSH levels continue to rise while estradiol levels fall like autumn leaves. These hormonal changes stabilize approximately two years after the FMP. So give your body a moment to find its new normal.
Following menopause, women enter the postmenopausal phase. Which is divided into early and late stages. With Early Postmenopause further subdivided into 3 sub-stages. Because apparently, we needed even more categories!
Stage +1: Early Postmenopause: (Early to mid 50’s)
- Stage +1a: (First year postmenopause) Welcome to the first 12 months after your final menstrual period, honey! Hormone levels, particularly estradiol, drop significantly. And I mean cliff-dive levels of dropping. This often leads to intense symptoms like hot flashes that could melt an ice sculpture. And night sweats that turn your bed into a water park. Women may begin experiencing changes in bone density and face an increased risk of cardiovascular issues. This is when you need to be extra vigilant about your health, sweetie!
- Stage +1b: (Second year postmenopause) During the second year, some women notice a decrease in the intensity of symptoms like hot flashes (hallelujah!). Hormone levels stabilize at lower levels as your body continues adjusting to the absence of menstrual cycles. Think of it as your body finding its sea legs on this new voyage.This period is crucial for focusing on bone health due to the increasing risk of osteoporosis. Calcium and vitamin D are your new best friends, darling!
- Stage +1c: (3 to 6 years postmenopause) By this stage, your body has largely adapted to postmenopausal hormone levels. Like a traveler adjusting to a new time zone. While vasomotor symptoms (those delightful hot flashes) may persist, they’re generally less severe.The focus shifts more prominently to long-term health concerns. Such as bone density loss and cardiovascular disease. Necessitating ongoing monitoring and preventive care. You’re not just managing symptoms anymore, honey. You’re investing in your future fabulousness!
Stage +2: Late Postmenopause: (Mid 50’s onwards) Duration: Remaining lifespan (the grand finale that never ends!)
This stage represents the remaining lifespan after menopause. Typically beginning in the mid-50s and extending for the rest of your magnificent life. Hormonal levels stabilize as your body adjusts to low levels of reproductive hormones. You’ve found your new normal, darling!
While menopausal symptoms usually subside (thank goodness!), aging-related issues become increasingly prevalent. Women may experience symptoms of genitourinary syndrome of menopause (GSM). That’s vaginal dryness, thinning of the vaginal lining, and urinary symptoms due to low estrogen levels. Not the most glamorous topic, but we’re keeping it real here, sweetie!
Although average FSH levels may decrease many years after menopause in very elderly individuals, this remains a high-risk phase for women. The decreased estrogen levels increase the risk of developing osteoporosis, cardiovascular disease (CVD), dementia, Alzheimer’s disease (AD), and cancer. This necessitates ongoing healthcare management to address these potential health concerns.
You’ve Got This, Darling
So there you have it. The STRAW+10 stages explained from start to finish. From your first period all the way through to late postmenopause, every twist, turn, and hormonal plot twist mapped out for you.
Here’s the beautiful truth: understanding these stages doesn’t make menopause easier, but it does make it less frightening. Because when you know where you are on the map, you can stop wondering “what the hell is happening to me?” and start asking “what do I need right now?”
And that, ma chérie, is everything.
You’re not lost. You’re not broken. You’re not imagining things. You’re simply moving through a natural transition that every woman experiences. And now you have the STRAW+10 system to prove it.
So take this knowledge, use it well, and remember: wherever you are on this journey, you’re exactly where you’re meant to be. And you’re handling it like the absolute legend you are.
Where to Go Next
If you want the full panoramic view of how all of this fits together, start with our complete STRAW+10: The Menopause Roadmap. It gives you the big picture in glorious detail.
And if you’re sitting there thinking, “Okay, but why is my body doing this? And why don’t my symptoms match my best friend’s?” Then you’ll want to explore Menopause Hormones or Symptoms by Stage alongside this page.